Managed Care Plan
Overview
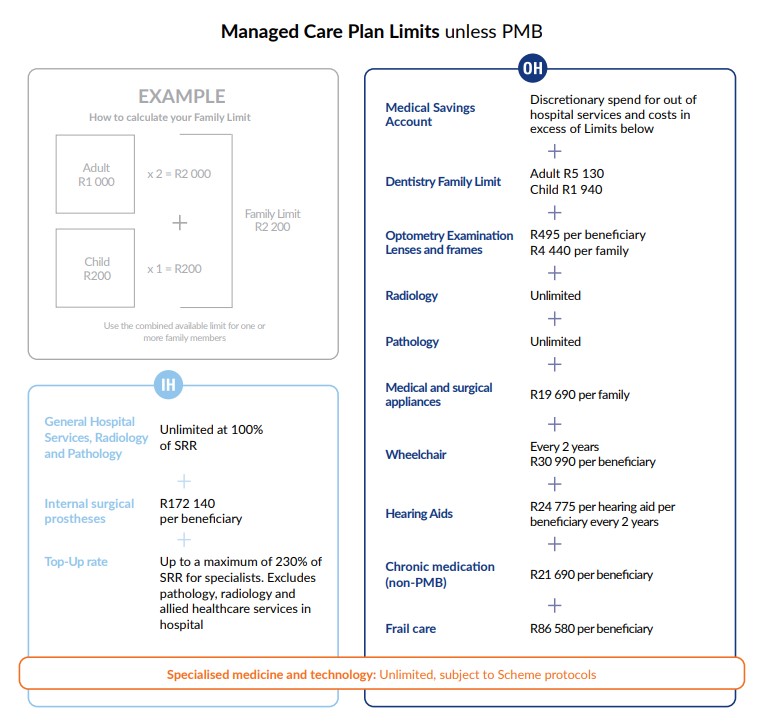
Managed Care Plan offers the following comprehensive benefits:
- Unlimited hospital cover paid at 100% of the Scheme Reimbursement Rate (SRR)
- The Top-Up rate pays up to a maximum of 230% of the SRR for non-network specialist services in hospital, excluding pathology, radiology, allied healthcare services and GPs performing specialist services (230% = 100% SRR + additional 130% of SRR)
- A Medical Savings Account for out of hospital services and discretionary spend
- Unlimited Radiology and Pathology
- Frail care where clinically required
- Extensive chronic medication
- Voluntary use of a GP network (no co-payments)
- Reimbursement for specialist consultations and procedures out of hospital up to 125% of SRR for non-network specialist services
Contributions are split as follows:
- 21% allocated to savings, for discretionary spend.
| Contributions (excluding savings) | ||
|---|---|---|
| Member | Adult dependant | Child dependant |
| R5 560 | R5 560 | R1 290 |
| Savings | ||
|---|---|---|
| Member | Adult dependant | Child dependant |
| R1 480 | R1 480 | R340 |
| Total contribution (including savings) | ||
|---|---|---|
| Member | Adult dependant | Child dependant |
| R7 040 | R7 040 | R1 630 |
*2025 benefits and contributions as approved by the Registrar for Medical Schemes.